Austerity and Health: Some Lessons from Around the World; Some Cautions for Saskatchewan
The People’s Health Movement – Canada (PHM‐C) agrees with the assessment of austerity’s failure as summarized by the Canadian Centre for Policy Alternatives (CCPA) in their December 2016 report The Futility of Austerity: Lessons for Saskatchewan. We would add that, even before the disastrous decade of austerity implementation proved to international financial institutions that austerity policies did not promote economic growth, overwhelming global evidence had illustrated that investments in health and education are inextricably linked to economic development (and growth). The evidence is clear: making such investments is sound economic policy.
Our submission to SaskForward is based on the work of the People’s Health Movement, a global network of grassroots health activists, civil society organizations and academic institutions guided by the goals and framework presented in The People’s Charter for Health (PHM 2000). The PHM’s Global Health Watch reports locate decisions and choices that impact health in the structure of global power relations and economic governance, and are widely perceived as the definitive voice for an alternative discourse on health. The most recent report in the series, Global Health Watch 4, was released in 2014. Our submission is also based on the thinking of several other major authors in the field, journal articles, reports, articles in the media, etc.
Public finance is a public health issue. Understanding how and why choices about the level and incidence of taxation and public expenditure affect health outcomes and health inequalities should be regarded as a core public health competence. Everywhere we observe it, austerity is selective – with resources continuing to be available for elite projects and agendas of questionable benefit, in equity terms in particular. As public health researchers, educators and practitioners we must therefore challenge the rhetoric of austerity and insist on health equity as a priority in public finance. (Schrecker 2017)
PHM‐C’s primary recommendation to SaskForward is that sustained or increased investments in publicly funded, equity‐based health programs and services are necessary to alleviate the undue suffering that Saskatchewan’s current economic crisis will continue to provoke, particularly among marginalized populations. Oppressed groups often suffer even more under austerity conditions as a results of budget cuts to particular programs, and for this reason we need to pay particular attention to the social determination of health (and ill‐health) among the Indigenous peoples of the province.
In this submission we make several observations of the observed effects of austerity on health outcomes, drawing from the experiences of countries in the European Union (EU) where austerity has been more extensively studied. We examine those effects more closely though an extreme case study of austerity (Greece). We then explore several current Canadian issues related to health care cuts, and end with considerations of the longer‐term impacts of austerity policies through the three policy interrogatives.
1. Who Are We?
Globally the People’s Health Movement operates in more than 70 countries. Within countries and regions, it operates to mobilize support for addressing global health crises caused by growing inequities within and among nations. This is accomplished through local and regional mobilizations, campaigns and awareness‐raising. At the global level the PHM’s major activities centre on watching, documenting and educating activists’ struggles for health; these include the WHO Watch, Global Health Watch publications and International People’s Health University (IPHU) teach‐ins. At the regional level issues and struggles vary and so do mobilizing strategies.
Within Canada we are a small network of concerned individuals and organizations linked primarily through a list‐serve and regular communications. While most of our activist work is undertaken through local initiatives – not necessarily identified as ‘PHM activities’ – we share the PHM’s global commitment to comprehensive primary health care and addressing the social, environmental and economic determinants of health. We also coordinate with and cooperate on issues and campaigns as part of the regional North America chapter. Our most recent regional event was a one‐day North America Regional People’s Health Assembly, held in August, in conjunction with the World Social Forum. More recently, PHM‐ Canada made a submission to the Expert Panel Review of Environmental Assessment Processes entitled Why We Need to Remember Health in This Conversation (PHM‐C 2016).
2. Overview: Causes of the Causes
In health terms, economic policies are often considered “the causes of the causes.” While they do not produce disease pathogens directly, they affect health by exposing particular groups of people to more or less risk, particularly but not solely, by their effects on social health determinants and health‐determining processes. Economic policies and trends can determine who gets or doesn’t get income supports and educational opportunities; they can also can determine who is “more likely to binge on alcohol, catch tuberculosis in a homeless shelter, or spiral into depression” (Stuckler and Basu 2013: 139).
Research linking economic policies and trends to health outcomes has suggested cumulative, unequal, and intergenerational effects. In an extensively cited research briefing by the UK organization Psychologists Against Austerity, for example, evidence shows that austerity policies can have damaging health effects intergenerationally with ”further problems … being stored for the future” (Psychologists against Austerity 2015). The latest research has begun to demonstrate plausible models for the epigenetic transmission of health responses to stress across generations, meaning our choices now that undermine the resilience of already vulnerable communities will have a social cost many decades into the future (Franklin et al 2010, Bowers and Yehuda 2016). We will discuss the health impacts of adverse childhood events in more detail later.
Numerous articles in reputable health journals document how the Great Financial Crisis which began in 2008 and the ill‐conceived austerity policies implemented in its wake have affected health both directly and indirectly. Directly, both health system and population health outcomes are affected and recorded in terms such as health system coverage, unmet health needs, health worker to population density, and morbidity, mortality and self‐ reported health status statistics and reports. Less direct effects are the effects of austerity policies on social determinants of health such as housing, income, food security and employment. While both direct and indirect effects can be studied, the PHM‐C suggests that assembling the case of ‘austerity and health’ requires both an understanding of the political economy of health and the kind of data that can provide for a robust analysis of trends.
To that end, the PHM‐C suggests that the more health and socio‐demographic data that is available, and the more detailed those data are (sufficient to allow disaggregation by gender, ethnicity, geographic location, etc.), the better able critical researchers and health activists will be able to track these trends. Accurate and detailed data allows for the production of solid evidence that can challenge the ideological positions often used to justify cuts to wages, programs and services.
3. Neoliberalism, Austerity and Health
According to analyst Richard Seymour, the popular representation of austerity as ‘short term spending cuts’ disguises its connection to the pernicious doctrine of neoliberalism, of which it is part and parcel. He suggests that rather than a simple set of policies to erase short‐term deficits under the auspices of austerity, we are seeing a fundamental neoliberal shift that includes: 1) a drastic long‐term ‘rebalancing’ of economies from consumption toward investment – or “away from wages and towards profits”; 2) growing strength of financial capital, and the corresponding spread of precariousness in all areas of life, most notably precarious work; 3) increased social inequality and stratification within classes; 4) growing fusion of the interests of states with that of corporations; 5) reorganization of the state from welfarist toward penal and coercive orientations; and, 6) dissemination of cultures which value hierarchy, competitiveness and “casual sadism toward the weak” (Seymour 2014, p. 3). Not all of these aspects of the shift are considered here, but are all inextricably linked to societal well‐being and would be useful to keep in mind in our collective analysis.
The PHM’s perspectives on the health crises of neoliberal globalization are set out in Chapter A1 of Global Health Watch 4. The chapter sets out a periodization and typology of three forms of neoliberalism:
- Neoliberalism 1.0: Structural adjustment
- Neoliberalism 2.0: Financialization
- Neoliberalism 3.0: AusterityWith regard to the third phase, austerity, the report notes that:The stunning failure of the 2008 crisis to delegitimize neoliberalism reveals the extent to which public policy had been influenced by the private sector (and primarily financial institutions). Neoliberalism was never about eliminating the state; instead, it was about occupying it, ‘a reconfiguring of both (state and market) so that they become thoroughly enmeshed.’ The ‘austerity agenda’ is merely one of the means of completing this phase of neoliberalism. Its key tenets differ little from those of Neoliberalism 1.0 … One key difference is that these policies are now a global phenomenon affecting high‐income countries as well. Contrary to widely held assumptions, however, this fiscal contraction is still most severe in the developing world.
and concludes that:
There is, in fact, robust evidence that every dollar in public spending can generate more than a dollar in economic growth in the ‘real economy’ of production and consumption, by purchasing goods and services that employ people, by employing people who purchase other goods and services, and by signalling stability to the private sector, which is then motivated to undertake its own increased activity. In the post‐[Global Financial Crises] environment, government spending is thought to have an average fiscal multiplier effect of 1.6. Recent estimates of European public spending by sector show much greater multiplier impacts for investments in health, education and environmental protection than, for example, in defence. Other data from Eurozone countries show that governments with higher rates of spending are recovering faster from the 2008 GFC. There is similar evidence available from the United States as well. Emergency unemployment benefits, extended by the US government in the wake of the GFC, are credited with reducing the economic impacts of the recession. These emergency benefits ended in December 2013 for 1.3 million Americans, which one economist estimated is costing the US economy US$1 billion a week, owing to decreased spending by the jobless.
Simply put, government spending in the health and social protection sectors is not only good for health equity and social stability, it is also good for the economy. Even the World Bank and the International Monetary Fund (IMF) have begun to accept the empirical evidence of the shortcomings of austerity, calling for government caution in implementing public sector cutbacks in recognition of the ‘fiscal multiplier’ effect of government spending.
The health‐harmful effects of austerity are being better documented and becoming more widely known. This evidence in itself provides health activists with strong arguments to reject austerity. Even by the standards of very mainstream economics, austerity simply does not make any sense. Say it loudly. Say it often.
4. Austerity and Health in the European Union (EU)
Perhaps more rigorously studied than other regions of the world, studies of the health effects of austerity regimes in the European Union (EU) have suggested that both national austerity policies specifically, and the legal obligation to adopt very low deficits that EU member states face have led to legal requirements for cuts to social spending. When imposed on health systems, these have translated as legal limits on health spending, with consequences for quality and access (Legido‐Quigley and Greer 2016).
As Schrecker and Bambra explained in their 2015 book How Politics Makes Us Sick: Neoliberal Epidemics, cuts to social spending and their effects have been not distributed evenly across societies. In describing the consequences of recent economic and social policies as ‘neoliberal epidemics’ they combined or conflated three categories: a health outcome of rising concern (obesity, one of many outcomes they could have chosen); key social determinants of health outcomes (economic inequality and insecurity); and a policy driver of those social determinants (austerity). Schrecker and Bambra felt that this conflation was justified because (a) an abundant evidence base connects inequality, insecurity and austerity with adverse health outcomes, of which obesity is only one; (b) the phenomena in question exist on such a scale and have spread so quickly across time and space that if they involved pathogens they would be seen as of epidemic proportions; and, (c) the epidemics in question are direct consequences of neoliberal economic and social policies.
Within vulnerable populations of European societies, increased stress due to economic hardship has resulted in marked increases in mental stress and depression (Psychologists Against Austerity 2015) and increased risk of initiating substance (alcohol, smoking, illicit drug) use (Dom et al 2016). Specific attention must be paid to the impact of austerity measures on rates of mental distress and suicide behavior over the life course. Recent research from Scotland has demonstrated that “The risk of suicide increased … for those born between 1960 and 1980, especially for men living in the most deprived areas, which resulted in a rise in age‐standardised rates for suicide among young adults during the 1990s. This is consistent with the hypothesis that exposure to neoliberal politics created a delayed negative health impact.” It is profoundly important to note that the impact of austerity policies were greatest on “men living in the most deprived areas” of Scotland. These path‐breaking findings follow on research which outlined the broader impacts of the neoliberal “political attack” on health in Scotland (Collins and McCartney 2011).
5. Greece: An Extreme Case Study
The effects of austerity on health in Greece have been studied intensely. Although Greece as a country has a socio‐economic context and health system that is distinct from Canada and Saskatchewan, the intensity of both the measures of austerity imposed after 2010, and the clear health effects experienced provide a cautionary tale.
In Greece, the financial crisis of 2008 led to successive rounds of austerity imposed by the Troika (the European Commission, the European Central Bank and the International Monetary Fund) as conditions for loans from the IMF. These conditions included drastic cuts to health care coverage, prevention and treatment for Greek citizens such as: the requirement of a cap of 6% GDP for expenditure on healthcare; reduction by 10% of public health expenditure on pharmaceuticals; cuts to hospital budgets and to harm reduction programs (1/3 of street health programs cut; syringe and condom distribution cuts of 10% and 24% respectively) and cuts to municipal budgets for public health activities (e.g. mosquito spraying programs). Cuts to mental health programs and coverage were also reduced 20% from 2010‐2011 and a further 55% from 2011‐2012 (Kentikelenis et al 2014).
Unsurprisingly, according to the Bank of Greece’s own admission, “the large cuts in public expenditure have not been accompanied by changes and improvements of the health system in order to limit the consequences for the weakest citizens and vulnerable groups of the society” (Bank of Greece 2016). Below is a short compendium of published health effects, trends and outcomes since the establishment of these policies:
- 35,000 clinician jobs slashed (Stuckler and Basu, 2013); 15% cuts in health worker salaries, 10% cuts in pensions; retirement age has increased from 65 to 67; about 1/3 of graduate nurses will remain unemployed for up to four years upon graduation; high levels of job dissatisfaction and burnout for nursing staff (Simou and Koutsogeorgou 2015). Between 2009‐2014, 120,000 mostly post‐graduate level university‐trained professionals had left Greece, among which were more than 3000 newly graduated doctors (Rodgers and Stylianou 2015).
- Increased health inequalities: the proportion of individuals on low incomes reporting unmet need due to cost doubled from 7% in 2008 to 13.9% in 2013, while the unmet need among the richest population quintiles decreased, leading to a ten‐ fold increase in the health gap between the rich and poor (Bank of Greece 2016; Karanikolos and Kentikelenis 2016).
- The prevalence of major depression increased from 3.3% in 2008 to 6.8% in 2009, to 12.3% in 2013 (Bank of Greece 2016; Economou et al 2016).
- Infant mortality increased nearly 50%; 19% increase in low‐birthweight babies between 2008 and 2010 (Kentikelenis et al 2014).
- Increase in chronic diseases increased approximately 24% (Kentikelenis et al 2014).
- In Southern Greece, a West Nile virus killed 62 people in 2010, and malaria returned after 40 years (due to cuts to mosquito spraying programs).
- Heroin use increase of 20%; tenfold increase in HIV cases in 2011, largely attributable to infected needles (Stuckler and Basu 2013).
These appalling changes in health outcomes have occurred in a country that is part of the European Union. While we in Saskatchewan will likely never experience the severity of these cuts and the magnitude of these changes in health outcomes, the Greek example clearly suggests the direction of direct health effects due to changes to health care systems, worker, coverage and programs in an austerity regime.
6. Canada
In Canada a steady slow erosion of public services spending starting with Paul Martin’s austerity budgets. In the Harper years, a slowing down of public share of total health spending was accomplished by not increasing the percentage of health spending to GDP ratio, which resulted in health transfers stagnating.
Fast forward: throughout December and January of 2016, after a failed attempt at a federal‐ provincial agreement regarding health transfers, provinces representing smaller populations – including Saskatchewan – began making bilateral agreements on transfers. This form of backroom bilateralism is flawed for several reasons:
- According to NDP health critic Don Davies, the side deals are divisive and break the spirit of ‘collaborative federalism’ and “end up posing a threat to the uniformity enshrined in the Canada Health Act.” For the Canadian Medical Association, “A national and strategic approach to improving our health care system remains essential” (Kirkup 2017).
- The federal government’s insistence on funding of mental health and home care, rather than allowing provinces to tailor a robust transfer to their own needs, is known globally as the vertical program approach to health funding. Authoritative sources have documented multiple countries where the approach has had a devastating effect on health systems worldwide, contributing to fragmentation of health systems (Kentikelenis et al 2014).
- Within Canada, perhaps more fundamentally, the formula for health transfers is questionable. The Canadian Health Coalition suggests have that“negotiations regarding the health transfer have missed the mark when it comes to addressing the needs of Canadians,” “While the negotiations have been centred on 3% or 6%, no one has been talking about how to ensure the funding can continue to deliver the services Canadians need. Tying the health transfer to GDP means that when the economy tanks and health care needs increase, there will be fewer dollars available.People without jobs and health benefits rely more heavily on the public system to meet their medical needs. We need funding that reflects the needs of Canadians, not the fluctuations of markets” (Canadian Health Coalition 2016).
Ottawa’s share of public health‐care spending, currently about 22 per cent, is set to fall to about 18 per cent within a decade (Yakabuski 2016).
We suggest that these current moves reflect the competitive, divide and conquer doctrine of neoliberalism, and set the stage for provincial governments to roll out and excuse their own policies under the blanket of austerity. As noted above, we in PHM Canada do not believe that clear trends in wealth concentration amongst the richest in the country that have emerged since the last round of austerity twenty years ago in Canada are unrelated to the dampened economic growth rates that we have experienced over the last decade. The most dynamic economies are those that support the spending of the poor and middle classes, who push supplemental income into the marketplace, rather than hoarding it as has been the tendency of the wealthy. These vibrant economies are more likely to support steady employment to a wide swathe of the population, with security and social conditions that support the well‐being and health of the whole community.
7. Policy Interrogative 1: What will be the direct and indirect health consequences if the current downturn in Saskatchewan’s economic situation is of a longer duration than the provincial government believes likely?
Austerity policies are often sold to the public as short‐term measures required to allow governments to manage fiscal pressures during a period of economic downturn, the assumption being that cuts can be reversed once robust economic growth resumes. Whether or not one agrees with this ‘belt‐tightening’ logic, there is another question that must be asked: what if global economic growth rates remain low, commodity prices remain low, and the pressure on the provincial government budget remains elevated?
In its latest economic outlook, released on January 16, the IMF estimates that Canada’s economy grew by just 1.3% in 2016, and is forecast to grow by 1.9% in 2017 and by 2.0 in 2018 – the same rates as for the ‘advanced economies’ as a whole. The IMF estimates just 1.6% annual real GDP growth for the ‘advanced economies’ in 2016, down from 2.1% in 2015 and down from its July 2016 forecast of 1.8%. (IMF 2017) This is primarily the result of the US having experienced the weakest economic recovery after a slump since the 1930s. Maurice Obstfeld, the IMF’s chief economist, has noted that “The crisis has left a cocktail of interacting legacies – high debt overhangs, nonperforming loans on banks’ books, deflationary pressures, low investment, and eroded human capital – that continue to depress potential investment levels” (Coy 2016).
Economic growth in the US is not forecast to rise beyond 2.5% in 2017 or 2018, and the IMF update notes that “there is a wide dispersion of possible outcomes around the projections, given uncertainty surrounding the policy stance of the incoming U.S. administration and its global ramifications.” That is far below the rate of 4% that US President Donald Trump has claimed that his proposed policies would achieve. ‘Trumponomics’ – tax cuts for corporations and the rich, private spending on infrastructure, and quantitative easing – may prove to be no more successful at generating economic growth than Japan’s ‘Abenomics’… although it may boost financial markets and launch a speculative boom. This is the reality of the world economy today.
If global – including Canada’s and Saskatchewan’s – economic growth rates stagnate, and if the province’s corporate taxes and royalty regimes are not increased, will Saskatchewan’s public health care system be slashed in the same way that Trump is planning to slash public health care in the US? What would be the direct and indirect health consequences to the people of the province, especially the least well‐off?
8. Policy Interrogative 2: Might the greatest impact of the provincial government’s austerity agenda be felt in decades to come, as a result of elevated rates of adverse childhood experiences?
There is an enormous body of evidence showing the negative health impacts of adverse childhood experiences (ACEs) over the life course. Two key studies in this regard are the Adverse Childhood Experiences study in the US [1] and the Christchurch Human Development Study (CHDS) in New Zealand. [2]
The US ACE’s overall findings were that there is “a strong graded relationship between the breadth of exposure to abuse or household dysfunction during childhood and multiple risk factors for several of the leading causes of death in adults.” (Felitti 1998)
Of specific relevance to economic policy is the ACE study’s publication which examined “the relation between eight types of adverse childhood experiences (ACEs) and three indicators of worker performance (serious job problems, financial problems, and absenteeism)” later in life: “Strong graded relations were found between the ACE Score (total number of ACE categories experienced) and each measure of impaired worker performance. We found strong evidence that the relation between ACE Score and worker performance was mediated by interpersonal relationship problems, emotional distress, somatic symptoms, and substance abuse” (Anda et al 2004). The authors concluded that: “The long‐term effects of adverse childhood experiences on the workforce impose major human and economic costs that are preventable. These costs merit attention from the business community in conjunction with specialists in occupational medicine and public health.”
The implications of the US ACE study and the CHDS are clear: spending cuts which put additional stress on families can result in children experiencing higher rates of ACEs. Higher rates of ACEs mean not only greater human suffering, but also higher demands on the health care system over the long term.
The alternative is to maintain – or increase – what American researcher Stephanie Seguino has termed social infrastructure investment, which “can in fact be self‐financing. This is because such expenditures, by promoting human well‐being, also raise economy‐ wide productivity, and stimulate development and growth. As a result, this type of spending stimulates an increase in taxable income in the future with which to finance the original costs of the expenditures. Thus, human development expenditures can create fiscal space, an effect that is more easily understood once we adopt a longer time horizon than is typically done” (Seguino 2016).
Seguino notes that research on ACEs “is an instructive example of the type of research that can help economists estimate the costs of “doing nothing” versus investing in ameliorating the lives of children through public spending on mental and physical health care, training for parents, as well as policies that improve the economic well‐ being of families.” She concludes: “These studies demonstrate that there are positive externalities to be had from publicly funding investments in what we might call the social infrastructure – the bedrock on which the entire economy is built. This is not to suggest that the purpose of social spending should be purely instrumental. Rather, it demonstrates that such spending is in fact mischaracterized as merely a cost. Research has demonstrated that social spending is affordable because of its effects on well‐being that have economy‐wide effects.”
Does the provincial government understand the life‐course impacts that austerity policies may have on the most marginalized members of our society? If so, how does it plan to protect the well‐being of vulnerable children as its cuts take effect?
9. Policy Interrogative 3: Will data of sufficient richness to allow detailed monitoring of the impact of austerity on health over time, disaggregated by geography and population cohorts, be made available to the public and to analysts?
Citizens are entitled to accurate and accessible data on the state of their society. Given the scale of the austerity measures which the provincial government may be about to implement, it is imperative that data systems of sufficient richness to allow detailed monitoring of the impact of austerity on health over time.
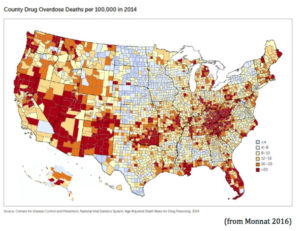
Recent research in the US has shown how changes in mortality and morbidity patterns have been structured by ethnicity, sex and age with “a marked increase in the all‐cause mortality of middle‐aged white non‐Hispanic men and women in the United States between 1999 and 2013” (Case and Deaton 2015). Data from the Centers for Disease Control and Prevention are available at the county level, which allows for nuanced understanding of epidemiological transition. For example:
Will data of sufficient richness to allow detailed monitoring of the impact of austerity on health over time, disaggregated by ethnicity, sex, age and geography, be made available to the public and to analysts? It will be especially important to be able to measure the impact of government austerity measures on indigenous peoples and other vulnerable sections of the population.
10. Conclusion
Austerity involves the redistribution of costs in society onto communities that already bear considerable burdens. With the rollback of the formal care sector, caregiving work – whether it be acute medical care or long‐term disability care – falls to individuals and families, where it is overwhelmingly women who do the work. As the demands of this increased caregiving load often falls onto women, their own health falls under strain. Often the last to seek care for themselves, many may find themselves in emergency situations. Migrant workers who may already feeling pressure from precarity may find their working conditions further eroded, thereby exacerbating chronic conditions, their health further compromised by racist violence whipped up by mythologies of scarcity. Indigenous peoples may find the obligations of health services to them under treaty law compromised by rhetoric about limited resources, when in reality, the long goal of neoliberalism under the guide of austerity is to distribute resources away from the vulnerable towards those with power.
References
Anda, Robert F., et al. (2004) “Childhood abuse, household dysfunction, and indicators of impaired adult worker performance.” The Permanente Journal 8:1. https://www.thepermanentejournal.org/files/Winter2004/childhood.pdf
Bank of Greece. (2016) Monetary Policy Report 2015‐2016. http://www.bankofgreece.gr/BogEkdoseis/NomPol20152016.pdf Cited at http://www.keeptalkinggreece.com/2016/06/16/austerity‐kills‐bank‐of‐greece‐ reports‐greeks‐health‐deteriorating‐life‐expectancy‐shrinks/
Bowers, Mallory E., and Rachel Yehuda. (2016) “Intergenerational transmission of stress in humans.” Neuropsychopharmacology Reviews 41. http://www.nature.com/npp/journal/v41/n1/abs/npp2015247a.html
Canadian Centre for Policy Alternatives. (2016) The Futility of Austerity: Lessons for Saskatchewan. https://www.policyalternatives.ca/publications/reports/sasknotes‐ futility‐austerity
Canadian Health Coalition. (2016 December 8) “Health care funding should be determined by need, not market fluctuations.” Media release. http://www.healthcoalition.ca/health‐ care‐funding‐should‐be‐determined‐by‐need‐not‐market‐fluctuations/
Case, Anne, and Angus Deaton. (2015) “Rising morbidity and mortality in midlife among white non‐Hispanic Americans in the 21st century.” Proceedings of the National Academy of Sciences 112:49. http://www.pnas.org/content/112/49/15078.full.pdf
Collins, Chik, and Gerry McCartney. (2011) “The impact of neoliberal ‘political attack’ on health: The case of the ‘Scottish effect’.” International Journal of Health Services 41:3. http://journals.sagepub.com/doi/abs/10.2190/HS.41.3.f
Couper, Sarah, and Phil Mackie. (2016) ‘Polishing the Diamonds’: Addressing Adverse Childhood Experiences in Scotland. Glasgow: Scottish Public Health Network. https://www.scottishrecovery.net/wp‐content/uploads/2016/06/ACE_Repor_‐ Final_2016.pdf
Coy, Peter. (2016 October 19) “Global markets stumble into a high‐debt, low‐investment 2017: Next year will be mediocre at best.” BloombergBusinessWeek. https://www.bloomberg.com/news/features/2016‐10‐20/global‐markets‐stumble‐ into‐a‐high‐debt‐low‐investment‐2017
Dom, Geert, et al. (2016) “The impact of the 2008 economic crisis on substance use patterns in the countries of the European Union.” International Journal of Environmental Research and Public Health 13:1. http://www.mdpi.com/1660‐4601/13/1/122/htm
Economou, Marina, Lily Evangelia Peppou, Kyriakos Souliotis, and Stelios Styliandis. “The impact of the economic crisis in Greece: Epidemiological perspective and community implications.” in: Styliandidis, Stelios (ed.) Social and Community Psychiatry: Towards a Critical, Patient‐Oriented Approach. Springer. http://dx.doi.org/10.1007/978‐3‐319‐ 28616‐7_24
Felitti, Vincent J., et al. (1998). “The relationship of adult health status to childhood abuse and household dysfunction.” American Journal of Preventive Medicine 14:4.
http://www.ajpmonline.org/article/S0749‐3797%2898%2900017‐8/abstract
Franklin, Tamara B., et al., (2010) “Epigenetic transmission of the impact of early stress across generations,” Biological Psychiatry 68:5. http://dx.doi.org/10.1016/j.biopsych.2010.05.036
International Monetary Fund. (2017 January 16) World Economic Outlook Update. http://www.imf.org/external/pubs/ft/weo/2017/update/01/pdf/0117.pdf
Karanikolos, Marina, and Alexander Kentikelenis. (2016) “Health inequalities after austerity in Greece.” International Journal for Equity in Health 15:1. http://dx.doi.org/10.1186/s12939‐016‐0374‐0
Kentikelenis, Alexander, Marina Karanikolos, Aaron Reeves, Martin McKee, and David Stuckler. (2014) “Greece’s health crisis: From austerity to denialism.” The Lancet 383:9918. http://dx.doi.org/10.1016/S0140‐6736(13)62291‐6
Kirkup, Kirsty. (2017 January 18) “Advocates call for holdout provinces to sign health transfer deals.” Canadian Press. http://www.ctvnews.ca/politics/advocates‐call‐for‐ holdout‐provinces‐to‐sign‐health‐transfer‐deals‐1.3246545
Legido‐Quigley, Helena, and Scott L. Greer. (2016) “Austerity, health, and the Eurozone.” International Journal of Health Services 46:2. http://journals.sagepub.com/doi/full/10.1177/0020731416637158
Monnat, Shannon M. (2015) “Drugs, death and despair in New England.” Communities & Banking Fall 2016. www.bostonfed.org/publications/communities‐and‐ banking/2016/fall/drugs‐death‐and‐despair‐in‐new‐england.aspx
Parkinson, Jane, et al. (in press) “Recent cohort effects in suicide in Scotland: A legacy of the 1980s?” Journal of Epidemiology & Community Health. http://jech.bmj.com/content/early/2016/07/18/jech‐2016‐207296.abstract
People’s Health Movement. (2000) The People’s Charter for Health. http://www.phmovement.org/en/resources/charters/peopleshealth
‐‐‐‐‐ (2014) Global Health Watch 4. http://www.ghwatch.org/node/45484
People’s Health Movement – Canada. (2016) Why We Need to Remember Health in This Conversation. Submission to the Expert Panel Review of Environmental Assessment Processes. http://eareview‐examenee.ca/wp‐ content/uploads/uploaded_files/phmceaareviewwhyweneedtorememberhealthinthisc onversation.docx.pdf
Psychologists Against Austerity. (2015) The Psychological Impact of Austerity: A Briefing Paper. https://psychagainstausterity.files.wordpress.com/2015/03/paa‐briefing‐ paper.pdf
Rodgers, Lucy, and Nassos Stylianou. (2015 July 16) “How bad are things for the people of Greece?” BBC News. http://www.bbc.com/news/world‐europe‐33507802
Schrecker, Ted. (2017) Personal communication.
Schrecker, Ted, and Clare Bambra. (2015) How Politics Makes Us Sick: Neoliberal Epidemics. Palgrave Macmillan UK.
Seguino, Stephanie. (2016) “The costs of inequality and the affordability of solutions.” Journal of Human Development and Capabilities 17:3. http://www.tandfonline.com/doi/full/10.1080/19452829.2016.1203029
Seymour, Richard. (2014) Against Austerity: How We Can Fix the Crisis They Made. Pluto Press.
Simou, Effie, and Eleni Koutsogeorgou. (2015) “Quality indicators for primary health care: A systematic literature review.” Journal of Public Health Management & Practice 21:5. http://journals.lww.com/jphmp/Abstract/2015/09000/Quality_Indicators_for_Primar y_Health_Care___A.19.aspx
Stuckler, David, and Sanjay Basu. (2013) The Body Economic: Why Austerity Kills. Basic Books.
Yakabuski, Konrad. (2016 March 28) “Provinces will feel the bite when it comes to health care transfers.” The Globe and Mail. http://www.theglobeandmail.com/opinion/provinces‐will‐feel‐the‐bite‐in‐health‐ transfers/article29388708/
NOTES
- https://www.cdc.gov/violenceprevention/acestudy/. The full range of publications from the ACE study are available at http://www.cdc.gov/violenceprevention/acestudy/outcomes.html, helpfully organized by the health outcomes studied.
- http://www.otago.ac.nz/christchurch/research/healthdevelopment/index.html. The articles, reports, books and book chapters describing what has been learned from study of the CHDS cohort are listed at http://www.otago.ac.nz/christchurch/research/healthdevelopment/publications/

